Dr. Brian E. Shiozawa was appointed by the President as Regional Director in Region 8 on December 2017. As Regional Director, he leads the Denver based office as the personal representative of the Secretary. Dr. Shiozawa ensures the Department maintains close contact with state, local, and tribal partners and addresses the needs of communities and individuals in Colorado, Montana, North Dakota, Utah and Wyoming.
Friday, December 22, 2017
HHS Region VIII News: New Regional Director, Brian E. Shiozawa, M.D.
Dr. Brian E. Shiozawa was appointed by the President as Regional Director in Region 8 on December 2017. As Regional Director, he leads the Denver based office as the personal representative of the Secretary. Dr. Shiozawa ensures the Department maintains close contact with state, local, and tribal partners and addresses the needs of communities and individuals in Colorado, Montana, North Dakota, Utah and Wyoming.
Labels:
Disparities Office,
Events
Oral Health America's Webinar Series: Collective Engagement
|
Labels:
Events
SAMHSA Funding Opportunity Announcement (FOA)
SAMHSA Funding Opportunity Announcement (FOA)
Offender Reentry Program
Apply Today!
Deadline: January 26, 2018
The Substance Abuse and Mental Health Services Administration (SAMHSA), Center for Substance Abuse Treatment (CSAT) is accepting applications for fiscal year (FY) 2018 Offender Reentry Program (ORP) grants.
The 2018 ORP program is to expand substance use disorder (SUD) treatment and related recovery and reentry services to sentenced adult offenders/ex-offenders with a SUD and/or co-occurring substance use and mental disorders. These individuals are returning to their families and community from incarceration in state and local facilities including prisons, jails, or detention centers (i.e., the population of focus).
The full 2018 ORP expansion announcement can be found on the SAMHSA website at FOA Number: TI-18-003. When you are searching for a funding opportunity on Grants.gov, use SAMHSA’s FOA number as the Funding Opportunity Number listed above.
Anticipated Number of Awards: Up to 16
Anticipated Award Amount: Up to $425,000
Length of Project: Up to 5 years
Applicants should be aware that funding amounts are subject to the availability of funds.
SAMHSA will be hosting a Pre-Application webinar on December 19, 2017, see the attached document. The webinar will provide information on how to submit applications to SAMHSA using the NIH eRA System, including application and registration processes, requirements and validations and the post-submission process.
Also, please check the website for any additional information pertaining to the FOA.
Labels:
Funding Opportunities
Thursday, December 21, 2017
Free Fare Friday
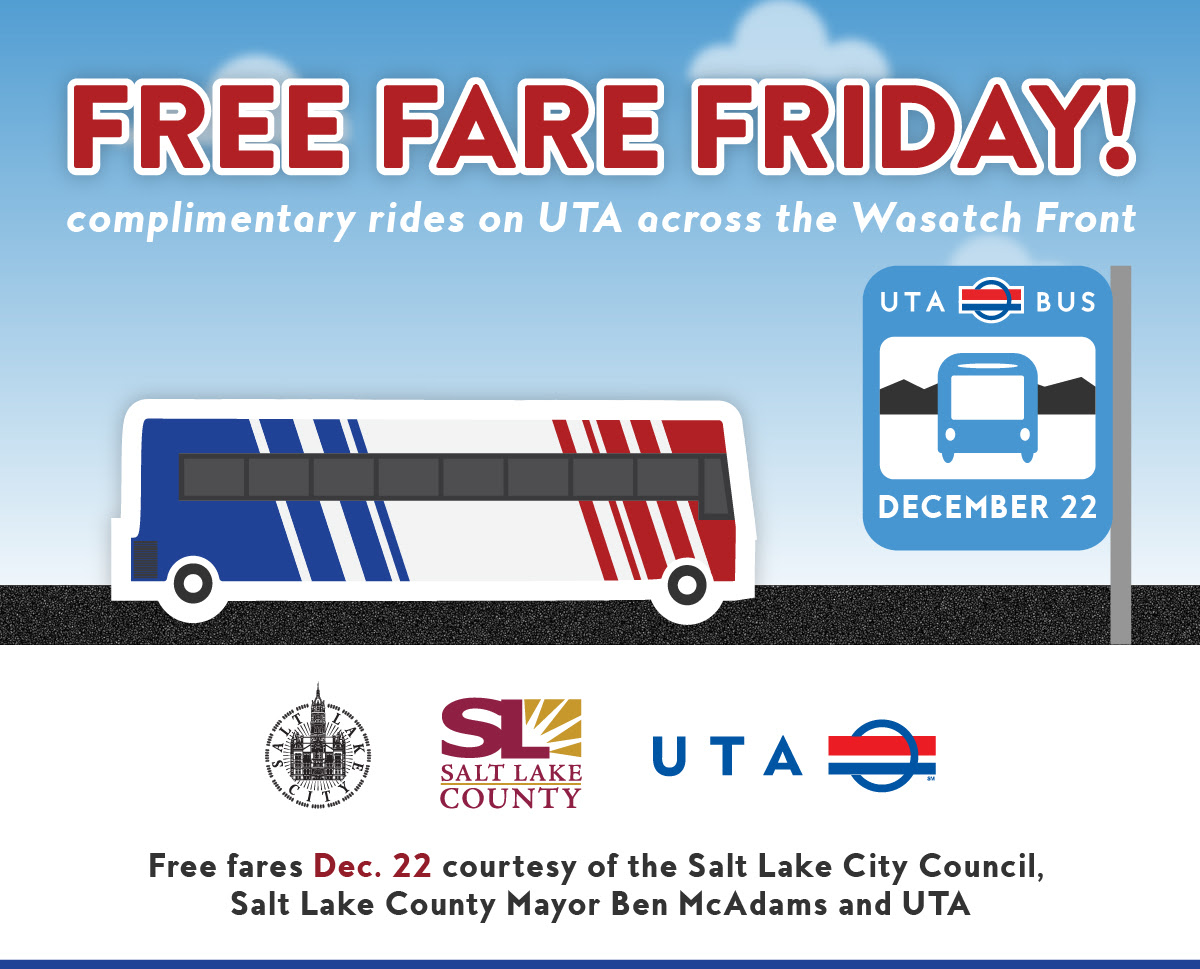
Free Fare to Help the Air
Enjoy complimentary rides on UTA across the Wasatch Front
this Friday, December 22 - all day!
New to public transit? Use UTA's Route Finder to plan your trip
The Salt Lake City Council, Salt Lake County Mayor Ben McAdams and Utah Transit Authority are teaming up to cover your fare all day on December 22!
By encouraging transit ridership, the partnership seeks to raise awareness of the opportunity to improve our wintertime air quality. Bus drivers will be instructed not to accept fares and TRAX/FrontRunner stations will have signs posted indicating that no fares are required.
The Council is proud to co-sponsor this Free Fare Friday. More info here.
Labels:
Events
Friday, December 15, 2017
Nearly 1 in 5 Utahns Live with a Disability
(Salt Lake City, UT) – According to a new report
released by the Utah Department of Health (UDOH), nearly one in five
(17.8%) Utah adults is living with a disability. The most common are
mobility-related disabilities (9.1%), followed by cognitive disabilities
(8.8%), disabilities that impact independent living (4.5%),
vision-related disabilities (2.8%), and disabilities that impact
self-care (2.3%). Data on deaf or hard of hearing were not included in
the report.
“Adults with disabilities experience significant differences in their health behaviors and overall health compared with adults without disabilities,” said Libby Oseguera, spokesperson with the UDOH. “Our data shows people with disabilities were more likely to engage in unhealthy behaviors like inactivity and tobacco usage and experience a higher incidence of chronic health conditions like diabetes and obesity.”
Many of the health outcomes that persons with disabilities are more likely to experience either contribute to the top causes of death or are one of the leading causes of death in the U.S. In fact, Utahns with disabilities were three times more likely to have a heart attack, two times more likely to be diagnosed with cancer (not including skin cancer), and two times more likely to have asthma or arthritis when compared to those without a disability. Focusing on improving health through exercise, proper nutrition, and preventive health check-ups often takes a backseat to the challenges faced in everyday life.
The report showed that among persons with disabilities:
Findings from the report also showed Utahns with disabilities were more likely to be female, Native American/Alaskan Native, and live in the Central Utah, Southeast Utah, Tooele County, or TriCounty local health districts. Persons with disabilities were also more likely to report lower education and income levels as well as a lack of health insurance when compared to those without disabilities.
“The Utah Department of Health recognizes these disparities and is working to make wellness and prevention more engaging and inclusive of people with disabilities in our programs, particularly those within our Bureau of Health Promotion,” said Kathy Paras, manager of the UDOH Disability and Health Program.
The report also provides a list of things the UDOH, healthcare providers, state officials and community leaders, and adults living with disabilities can do to improve health outcomes. Included is the recommendation to participate in Living Well workshops offered across the state that can help with management of chronic pain and chronic diseases, found at http://livingwell.utah.gov.
A copy of the report can be found at https://health.utah.gov.
# # #
Media Contact:
Libby Oseguera
(o) 801-538-6408
laoseguera@utah.gov
“Adults with disabilities experience significant differences in their health behaviors and overall health compared with adults without disabilities,” said Libby Oseguera, spokesperson with the UDOH. “Our data shows people with disabilities were more likely to engage in unhealthy behaviors like inactivity and tobacco usage and experience a higher incidence of chronic health conditions like diabetes and obesity.”
Many of the health outcomes that persons with disabilities are more likely to experience either contribute to the top causes of death or are one of the leading causes of death in the U.S. In fact, Utahns with disabilities were three times more likely to have a heart attack, two times more likely to be diagnosed with cancer (not including skin cancer), and two times more likely to have asthma or arthritis when compared to those without a disability. Focusing on improving health through exercise, proper nutrition, and preventive health check-ups often takes a backseat to the challenges faced in everyday life.
The report showed that among persons with disabilities:
- 36.9% report “fair” or “poor” health compared to only 6.7% among persons without a disability
- 41.9% report having seven or more days of poor mental health compared to 10.9% among persons without a disability
- Nearly half (49.9%) had a diagnosis of depressive disorder compared with 15.5% among persons without a disability
Findings from the report also showed Utahns with disabilities were more likely to be female, Native American/Alaskan Native, and live in the Central Utah, Southeast Utah, Tooele County, or TriCounty local health districts. Persons with disabilities were also more likely to report lower education and income levels as well as a lack of health insurance when compared to those without disabilities.
“The Utah Department of Health recognizes these disparities and is working to make wellness and prevention more engaging and inclusive of people with disabilities in our programs, particularly those within our Bureau of Health Promotion,” said Kathy Paras, manager of the UDOH Disability and Health Program.
The report also provides a list of things the UDOH, healthcare providers, state officials and community leaders, and adults living with disabilities can do to improve health outcomes. Included is the recommendation to participate in Living Well workshops offered across the state that can help with management of chronic pain and chronic diseases, found at http://livingwell.utah.gov.
A copy of the report can be found at https://health.utah.gov.
# # #
Media Contact:
Libby Oseguera
(o) 801-538-6408
laoseguera@utah.gov
Labels:
Data and Reports
UDOH Early Childhood Utah Program Manager Position open
 The Department of Health has an opening for an Early Childhood Utah Program Manager, posting # 14366. The posting will close at 11:59 PM on December 25, 2017 MST
The Department of Health has an opening for an Early Childhood Utah Program Manager, posting # 14366. The posting will close at 11:59 PM on December 25, 2017 MSTIn order to be considered for an interview for these positions, you will need to apply on-line at STATEJOBS.UTAH.GOV . If you have not done so already, you will need to create a job seeker account.
Labels:
Jobs
Salt Lake County Board Vacancies
Boards
and Commissions Update 12.13.17
Board
Openings:
We are currently seeking applicants and
recommendations for the following SLCO Boards and Commissions:
Housing
Trust Fund Advisory Board 10 vacancies
Purpose: To
address the concerns for affordable and special needs housing within the
county. To the extent possible, members shall include residents of each county
council district with at least four members having expertise in affordable
housing or special needs housing. Remaining members shall have expertise in the
areas of business, real estate, or housing development.
SLCO Fair
Board 5
vacancies
Purpose: To
enhance the interest of the community by establishing, conducting, and
maintaining fairs and exhibitions within Salt Lake County.
Vacant seats with the following areas of interest
are available: Volunteers, Business, Special Events (2 seats), Competitive
Exhibits.
Interested applicants should apply online at:
and/or contact Tiffany Clason at tclason@slco.org
or 385-468-7026.
Labels:
Events
Wednesday, December 13, 2017
America's Health Rankings from United Health Foundation shows Utah jumped to #4 in Healthiest States
The United Health Foundation 2017 Annual Report of America's Health Rankings looks at 35 different factors affecting people's health including rates of smoking, obesity, physical inactivity, low birth weight, drug deaths, environmental conditions like air pollution, and the number of doctors, dentists, and mental health providers per 100,000 people in their state.
Florida and Utah experienced the largest rank improvements since last year, rising four places in the rankings to No. 32 and No. 4 in the country, respectively. Florida’s improvements include positive changes in its rankings for the percentage of children in poverty and frequent mental distress since 2016. Utah also improved its rankings for several measures in the same time period, including air pollution and immunizations among children.
MORTALITY RATES ARE INCREASING IN MANY STATES, EVEN THOSE RANKED HIGHLY FOR OVERALL HEALTH
WIDE VARIATION ACROSS THE COUNTRY IN THE CONCENTRATION OF HEALTH CARE PROVIDERS
Utah and Idaho have fewer the 100 Primary Care Physicians per 100,000 population.
Read the entire 2017 report at United Health Foundation American's Health Rankings webpage.
Labels:
Data and Reports,
Disparities Office,
Events
Tuesday, December 12, 2017
Native Hawaiian and Pacific Islander National Health Interview Survey: Data Collection in Small Populations
The Native Hawaiian and Pacific Islander National Health Interview Survey: Data Collection in Small Populations
The National Center for Health Statistics at the Centers for Disease Control and Prevention released data from the Native Hawaiian and Pacific Islander (NHPI) National Health Interview Survey (NHIS) which was jointly supported by the Office of Minority Health at the U.S. Department of Health and Human Services (HHS). This project is the first national health survey to use a sample frame consisting of NHPI households. This project was the result of years of advocacy by Asian American, Native Hawaiian, and Pacific Islander community organizations, leaders, and health researchers, combined with advancements in federal policies on data collection standards for racial/ethnic populations. Please view the survey here.
The National Center for Health Statistics at the Centers for Disease Control and Prevention released data from the Native Hawaiian and Pacific Islander (NHPI) National Health Interview Survey (NHIS) which was jointly supported by the Office of Minority Health at the U.S. Department of Health and Human Services (HHS). This project is the first national health survey to use a sample frame consisting of NHPI households. This project was the result of years of advocacy by Asian American, Native Hawaiian, and Pacific Islander community organizations, leaders, and health researchers, combined with advancements in federal policies on data collection standards for racial/ethnic populations. Please view the survey here.
Labels:
Data and Reports
Wednesday, December 6, 2017
FOR IMMEDIATE RELEASE
December 5, 2017
- - - - -
Mayor Biskupski applauds Salt Lake City Council on action to address affordable housing
Today, the Salt Lake City Council took action on two proposals presented by the Administration to address the affordable housing crisis in Salt Lake City. The proposals specifically dealt with approximately $21 million-dollars of Redevelopment Agency (RDA) funding the RDA Board set aside to deal with affordable housing in the City.
The proposal prioritizes $10 million-dollars of funding to be administered by the RDA for a competitive fund available to developers and community groups interested in building affordable housing projects. $3 million-dollars will also be directed to the City’s Housing Trust Fund, administered by the City’s Housing and Neighborhood Development Division, to be used for general purposes and a Renovation Pilot Program, to incentivize owners to improve existing affordable housing options. The proposal also sets aside funding for specific projects, including the Barnes Bank Exchange project, and the redevelopment of the Capitol Motel.
“I am thrilled we are moving forward on funding innovative initiatives to address the affordable housing crisis in Salt Lake City, which align with our proposed housing plan, Growing SLC” said Mayor Jackie Biskupski on the proposal. “Today’s move demonstrates that both the City Council and I are in agreement that now is the time to aggressively move to bring units online quickly. This is the product of almost a year of hard work, dialogue, and collaboration to find a workable solution.”
Earlier this year, the Biskupski Administration provided the City Council with two proposals for the use of set aside funding, including one option to fund specific RDA projects and one option utilizing the City’s existing Housing Trust Fund. In working through the proposals, the Council created the $10 million-dollar RDA fund, while also funding aspects of the Housing Trust Fund option. The Mayor noted that the decision preserved the opportunity to fund projects which could create deeply affordable housing prior to the 2019 closure of the downtown shelter.
“My priority has been, and continues to be, on ensuring we have the necessary housing options available to make the new homeless resource center model a success,” said Mayor Biskupski. “When we focus on the face of this crisis, including those moving from homelessness and those just struggling to get by in our City, we are able to achieve great things.”
The proposal would give the RDA a greater role in affordable housing initiatives in the City, while enhancing the City’s existing funding options. The RDA is a division of the Department of Economic Development, which was created by the Mayor in 2016 to help streamline economic activity in the City.
“The vitality of the City is dependent on the principle of equity, from job to housing opportunities. Salt Lake City thrives when our residents have access to affordable housing that allows them to live where they work and enjoy the amenities where they call home,” said Lara Fritts, Director of the Department of Economic Development and CEO of the RDA. “The City’s economic development efforts, and the work being done by our team and Mayor, are enhanced by the Council’s decision today.”
The Council also asked the Administration to explore options for an incentivized inclusionary zoning policy. In November, HAND launched a public engagement survey regarding inclusionary zoning in the City. The survey is available at www.slcgov.com/hand.
#####
Contact:
Matthew Rojas
Labels:
Income Disparities
Monday, December 4, 2017
Learning and Growing: Healthy Development During Childhood and Adolescence Webinar
Learning and Growing: Healthy Development During Childhood and Adolescence – A Healthy People 2020 Progress Review Webinar New!
Register Now | December 12, 2017 | 12:30 to 2:00 p.m. ET
| Spread the word! Tell your colleagues and friends about this great learning opportunity. Forward this email or tweet about the webinar. |
Join us on Tuesday, December 12 at 12:30 p.m. ET for a Progress Review webinar featuring 2 Healthy People 2020 topic areas:
- Early and Middle Childhood
- Adolescent Health
You'll also learn how the City of Cincinnati Health Department is taking a comprehensive approach to providing school-based health services.
About Early and Middle Childhood & Adolescent Health
Childhood and adolescence provide the physical, cognitive, and social-emotional foundation for lifelong health, learning, and well-being. The behavioral patterns established early in life help determine young people's current health and well-being and their ability to live healthy and productive lives throughout their lifespan.
About Progress Review Webinars
The Progress Review webinars focus on tracking and measuring the progress of select Healthy People 2020 objectives throughout the decade.
Labels:
Data and Reports,
Events
Friday, December 1, 2017
Fluoride in Practice: Resources from the Association of State and Territorial Dental Directors
|
|
Labels:
Data and Reports,
Healthcare Access
Thursday, November 30, 2017
Announcing New Wellness Court Publication: Tribal Healing to Wellness Courts Treatment Guidelines
Tribal Healing to Wellness Courts: Treatment Guidelines, 2nd ed. (2017), is designed to provide tribal communities with an overview of Western substance abuse treatment strategies that have been developed by drug court programs over the past several years and that tribal programs might consider adapting, along with traditional healing practices. This guideline draws upon drug court standards and best practices, and the experiences of hundreds of tribal and state adult and juvenile drug court programs, operating in various environments and serving a wide range of individuals addicted to alcohol and/or other drugs. Tribal Healing to Wellness Courts: Treatment Guidelines for Adults and Juveniles (2002 draft).
You can find this publication for free download on our Tribal Healing to Wellness Court Publication Series webpage, as well as on our Home.TLPI.org website. The Tribal Healing to Wellness Court Publication Series is a free resource available to the field, documenting best practices and the latest in practice-based knowledge.
Labels:
American Indians,
Data and Reports
Wednesday, November 29, 2017
CMS posts update to Medicare Part D Opioid Prescribing Mapping Tool
The Centers for Medicare & Medicaid Services (CMS) released an updated version of the Medicare Part D opioid prescribing mapping tool. The mapping tool is an interactive, web-based visualization resource that presents geographic comparisons- at the state, county, and ZIP code levels - of Medicare Part D opioid prescribing rates. It allows users to understand and compare opioid prescribing at the local level and better understand how this critical issue affects communities across the country.
The updated version of the mapping tool presents Medicare Part D opioid prescribing rates for 2015 as well as the change in opioid prescribing rates from 2013 to 2015. New for this release is additional information on extended-release opioid prescribing rates, which have been associated with misuse, including both addiction and overdose deaths as well as analyses that identify county-level hot spots and outliers. In total, for Medicare Part D, there were approximately 80 million opioid claims for 111 distinct opioid products in 2015, accounting for $3.5 billion in spending.
The updated Medicare Part D Opioid Prescribing Mapping Tool can be accessed at:https://www.cms.gov/
Labels:
Data and Reports
Opioid Prescribing: Safe Practice, Changing Lives
Date: Thursday, December 14, 2017 | Time: 12:00pm (ET) to 3:00pm (ET)| REGISTER HERE!
DESCRIPTION: We now know that overdoses from prescription opioids are a driving factor in the 15-year increase in opioid overdose deaths. Since 1999, the amount of prescription opioids sold in the U.S. has nearly quadrupled, yet there has not been an overall change in the amount of pain that Americans report. This comprehensive course, developed by experts from Collaborative for REMS Education (CO*RE), incorporates all six units outlined in the FDA blueprint for safe opioid prescribing. Attend this webinar if you want to be able to:
· Counsel patients and caregivers about safer use of opioids;
· Describe strategies for diagnosing and managing opioid-addicted patients; and
· Practice techniques for safe opioid prescribing.
Labels:
Events,
Healthcare Access,
Training
Monday, November 27, 2017
FEMA Webinar: Tribal Individual Community Preparedness and Hazard Mitigation
Federal Emergency Management Agency
Intergovernmental Affairs Division
This month, FEMA will host a webinar on Tribal Individual Community Preparedness and Hazard Mitigation. The webinar will be on Wednesday, November 29, 2017 from 3-4 p.m.
For more information, please contact the Tribal Partners Branch at FEMA-IGA@fema.dhs.gov. For more information on how we engage and work government-to-government with federally recognized tribes and tribal executives, visit FEMA Tribal Affairs.
If you have any questions, please contact FEMA Intergovernmental Affairs at 202-646-3444.
Tuesday, November 21, 2017
New Diabetes Fact Sheets Available in English and Spanish

|
Labels:
Data and Reports,
Hispanics/Latinos
Pain in the Nation: The Drug, Alcohol and Suicide Epidemics and the Need for a National Resilience Strategy

New Report: Utah's Drug, Alcohol and Suicide Death Rate Could Increase 41 percent in Next Decade; Utah Would have 14th Highest Rate in Country
Study Highlights Solutions, Calls for National Resilience Strategy
Washington, D.C., November 21, 2017 – Utah's drug, alcohol and suicide death rate could increase by 41 percent in the next 10 years, according to a new report, Pain in the Nation: The Drug, Alcohol and Suicide Epidemics and the Need for a National Resilience Strategy, released today by the Trust for America's Health (TFAH) and Well Being Trust (WBT).
Utah's rate could rise to 70 per 100,000 deaths from these three causes by 2025 – which would be the 14th highest – compared to the state's current rate of 49.7 per 100,000 (as of 2015), which is the 15th highest.
Nationally, deaths from drugs, alcohol and suicide could account for 1.6 million fatalities over the coming decade (2016 to 2025). This would represent a 60 percent increase compared to the past decade, if recent trends hold, based on an analysis conducted by the Berkeley Research Group (BRG) for this report. From 2006 to 2015, there were 1 million deaths from these three causes.
- Nationally, in 2015, there were 127,500 deaths from drugs, alcohol and suicide. The epidemics currently are responsible for 350 deaths per day, 14 per hour and one every four minutes.
- According to the report's projections, this could reach 192,000 per year by 2025 (39.7 deaths per 100,000 in 2015 compared to 55.9 per 100,000 in 2025).
- At a state level, in 2005, 21 states and Washington, D.C. had death rates from these three causes above 30 per 100,000, and only six states had death rates above 40 per 100,000.
- As of 2015, 48 states and Washington, D.C. had rates above 30 per 100,000, 30 were above 40 per 100,000 and five states had rates above 60 per 100,000, including New Mexico which had the highest rate of 77.4 per 100,000.
- By 2025, 26 states could reach 60 deaths per 100,000 – and two states (New Mexico and West Virginia) could reach rates of 100 deaths per 100,000.

The study found, however, that these numbers may be conservative, especially with the rapid rise of heroin, fentanyl and carfentanil use. If the nation continues along recent trajectories, death rates would actually double to 2 million by 2025.
"These numbers are staggering, tragic – and preventable," said John Auerbach, president and CEO of TFAH. "There is a serious crisis across the nation and solutions must go way beyond reducing the supply of opioids, other drugs and alcohol. Greater steps – that promote prevention, resiliency and opportunity – must be taken to address the underlying issues of pain, hopelessness and despair.
Labels:
Data and Reports
Monday, November 20, 2017
Continuous Improvement Capacity Building Grants for agencies working with youth in South Salt Lake and Kearns
Continuous Improvement
Capacity Building Grants
funded by Regence
BlueCross BlueShield of Utah
Application
DEADLINE: December 01, 2017
United Way of Salt Lake (UWSL) has made a
commitment to the community to dramatically improve outcomes for every child in
our region. We believe that if
nonprofits, schools, post-secondary institutions, businesses, government,
philanthropies, and community members can align their resources toward the same
goals, we can eliminate disparities and ensure that every child achieves their
goals.
In partnership with Regence BlueCross
BlueShield, we invite you to apply for a Continuous
Improvement Capacity Building grant.
The goal of this grant is for selected nonprofits to measurably improve
an outcome for a group of targeted individuals through the implementation of
continuous improvement principles and increased staff capacity focused on
mental health for students and families in the Granite School District. Grant
recipients will receive the following:
1.
Two workshops exclusively for grant recipients
on results-based accountability and short-cycle continuous improvement
2.
Access to Results-Based Facilitation Training
and Leadership Training
3.
Two technical assistance sessions to ensure
clear implementation of outcome focused strategies
4.
A one-time grant of $5,000 to participate in
workshops and trainings and to implement a continuous improvement strategy
Nonprofits who provide mental health services
low to moderate income families in Granite School District in the below areas
are eligible to apply for the grant:
●
South Salt Lake
●
Kearns
Application Deadline: December 1, 2017.
Announcement of grant decisions will be made
by December 15, 2017.
If you have questions regarding this grant
application, please email Katherine Bark at katherine@uw.org. Get the grant application here.
Please send your completed application
electronically to:
Katherine Bark
Grants Manager
United Way of Salt Lake
Labels:
Funding Opportunities
Free, Online Trainings in Health Literacy
Even people who read well and are comfortable using numbers face health literacy issues when they aren’t familiar with medical terms or how their bodies work, when they have to interpret statistics and evaluate risks and benefits that affect their health and safety, or when they are voting on an issue affecting the community’s health and relying on unfamiliar technical information.
Trainings in health literacy, plain language, and culture and communication are essential for anyone working in health information and services. To make information more accessible and understandable to your audiences, consider taking online CDC trainings. (Continuing education credits and certificates are available.)
Choose from Five Different Trainings
Whether you are new to these topics, need a refresher, or want to train your entire staff, these courses are a good place to start:
- Health Literacy for Public Health Professionals (free continuing education)
- Writing for the Public (printable completion certificate)
- Using Numbers and Explaining Risk (printable completion certificate)
- Creating Easier to Understand Lists, Charts, and Graphs (printable completion certificate)
- Speaking with the Public (printable completion certificate)
Learn more about these trainings and visit CDC’s health literacy website for more information
Labels:
Data and Reports,
Events,
Training
Subscribe to:
Posts (Atom)




